
For something that is so natural and timeless, the menstrual cycle has surely taken a lot of interest and contention – many times causing ostracism and anguish spanning millennia. There are plenty of reasons why people may be interested in learning about the menstrual cycle. People may be experiencing their first ‘periods’, figuring out a method of birth control that works for them, considering family planning, diving deep into menstrual health research, or simply trying to understand the complexities of the reproductive tract.
Regardless of your Why, having a deeper appreciation for your body’s ability to go through different (hormonal) phases by design and purpose can be empowering. You can become more independent in making decisions about not only your reproductive health (such as preventing pregnancies and/or conceiving) but also your overall experience of health and well-being.
What you will learn in this article
- Your periods are not the same as your menstrual cycles. Your periods are periodic or regular menstrual bleeds.
- Your menstrual cycle is a more complex hormonal process (that includes your periods) that prepares your body for the possibility of pregnancy. (Believe it or not, our bodies are designed to conceive.)
- The brain, ovaries, and uterus are the primary organs involved in the menstrual cycle and they are constantly communicating via hormonal feedback systems.
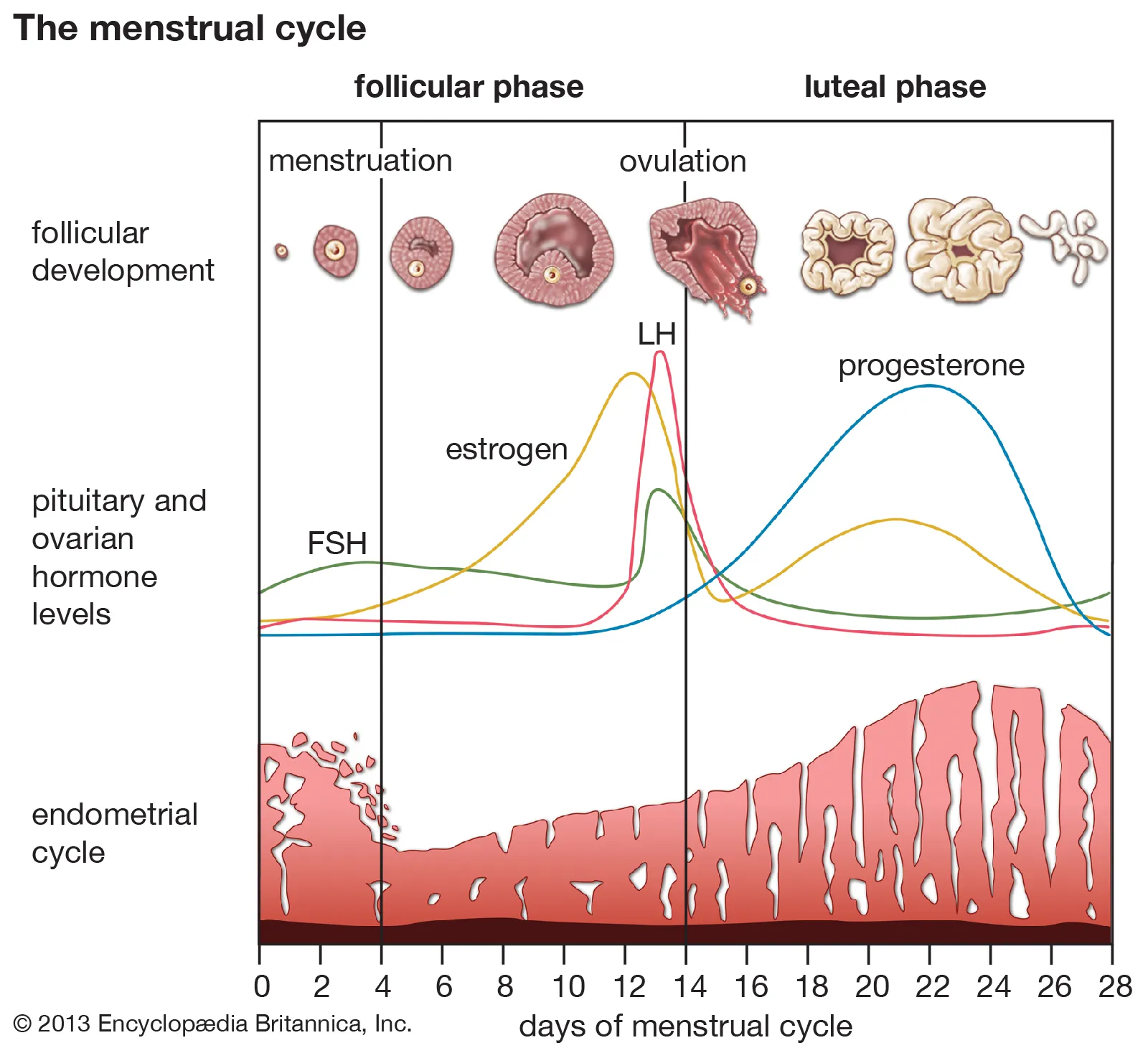
- The menstrual cycle is best studied by observing the ovaries and uterus and the phases they go through – The Ovarian Cycle and The Uterine Cycle.
- Ovulation, the release of an egg from a follicle, is the main event in the menstrual cycle. This event is the driving force of physiological changes in the ovaries and uterus.
- Your brain produces hormones Follicle Stimulating Hormone (FSH) and Luteinizing Hormone (LH) to initiate ovulation.
- In response to FSH, your eggs produce Estrogen during the Follicular Phase. Meanwhile, with Estrogen present, endometrial cells are proliferating (Proliferative Phase).
- High estrogen levels and the surge of LH levels trigger ovulation.
- After ovulation occurs and the egg disintegrates, the Corpus Luteum produces Progesterone in the Luteal Phase.
- Once progesterone production ceases, the uterine lining is shed, accompanied by bleeding. This process is menstruation, and it commences the new menstrual cycle.
- Beyond your brain, ovaries, and uterus, other bodily functions such as cervical mucus production and body temperature, are affected by hormonal changes in the menstrual cycle too.
- Menstrual cycles DO NOT need to be accompanied by debilitating premenstrual symptoms, cramping, pain, irritability, depression, bloating, heavy bleeding, unpredictability, and other discomforts.
- It is important to be aware of and seek urgent medical care for signs and symptoms of potentially serious reproductive health emergencies.
The menstrual cycle is more than just a period.
Are periods the same as menstrual cycles?
The short answer is – No, they are not the same.
The long answer is that what we familiarly know as our ‘period’ does not wholly encapsulate the intricacy of the menstrual cycle.
Your ‘periods’ are menstrual bleeds that occur periodically or in a regular monthly pattern. Your periods are a part of your menstrual cycle. On the other hand, your menstrual cycle is a more complex process orchestrated by interactions between your body’s tissues, cells, and hormones. It is a series of physiological events, including your menstrual bleeds, that occur regularly in preparation for the possibility of fertilization and pregnancy. (Whether or not you want to conceive, our bodies are designed for this purpose).
Your brain, ovaries, and uterus are constantly communicating
Throughout your reproductive life, your brain is in constant communication with your ovaries and uterus, and vice versa. They operate via impressively efficient feedback systems and hormones. To understand these hormonal feedback systems it may help to study what goes on between your brain, ovaries, and uterus in phases.
The menstrual cycle can be best studied in phases.
Because menstrual cycles primarily overtly impact the uterus and ovaries, your cycles are also sometimes described as ovarian cycles and uterine cycles respectively. The ovarian and uterine cycles are further broken down into phases. Different events occur during each phase, and these phases are facilitated by the brain. So, first let’s understand your brain’s role in your menstrual cycle.
Your brain
Your brain’s job is to initiate the process of getting your ovaries and uterus ready for a possible pregnancy. For a few days, a part of your brain called the anterior pituitary gland produces the hormone called Follicle Stimulating Hormone (FSH). FSH, from the name itself, stimulates the follicles in your ovaries to grow until ovulation occurs. There is another hormone that the anterior pituitary gland makes called the Luteinizing Hormone (LH), which shows up a little later in the first half of your cycle. LH builds up in your circulation and eventually helps to trigger ovulation. Ovulation, as you’ll learn later, is the main event of the menstrual cycle wherein an egg is released from the follicle and out of the ovary.
Your brain (anterior pituitary gland) ultimately produces hormones or dials back on hormone production depending on the levels of estrogen and progesterone produced by your ovaries – hence, the feedback system!
Quick hormone recap 1:
Your brain produces the Follicle Stimulating Hormone (FSH) and Luteinizing Hormone (LH).
Your ovaries: The Ovarian Cycle
The same hormonal feedback system that your brain is part of also influences how your ovaries respond. The ovaries go through three different phases throughout your menstrual cycle.
- Follicular Phase, which occurs before ovulation
- Ovulation, which happens when an ovum (egg) is released from an ovary, and
- Luteal Phase, which occurs after ovulation
Follicular Phase – The Race to Ovulation
In the beginning of your menstrual cycle (from cycle day 1 or the first day of your period until your period ends), the activity level within the ovaries is relatively quiet. Under the influence of FSH, you have a few follicles that will be ‘selected’ to develop – around 15 to 20 eggs start to mature in each ovary – until a Dominant Follicle (The Chosen Egg)* is selected for Ovulation. Recall that your eggs come in its own individual follicle. That is, your follicles kind of look like little sacs that each carry an egg.
As the race to ovulation happens, with FSH, your follicles are stimulated to produce estrogen. Estrogen production continues until ovulation occurs.
The follicular phase on average takes about two (2) weeks. Realistically, it can take anywhere from about 8 to 21 days, sometimes longer, before ovulation happens.
Ovulation – The Main Event of Your Cycle
Ovulation, which is the release of an egg from a follicle, is the main event in the menstrual cycle. This event is the driving force of physiological changes in the ovaries and uterus. The high levels of estrogen will also be picked up by your pituitary gland and will consequently have an abrupt surge of luteinizing hormone (LH). With the levels of estrogen increasing (which is also referred to as peak estrogen levels) and the surge in LH levels, ovulation eventually occurs when one ovary releases an egg from the most dominant follicle.
Once the egg is released from the Dominant Follicle during Ovulation, it can potentially be fertilized by sperm. If the egg does end up being fertilized, the fusion of egg and sperm becomes a zygote. As the single-celled zygote makes its way to the fallopian tube and the uterus, it goes through fascinating cellular processes eventually becoming an embryo, and implants into the uterine lining, resulting in a pregnancy.
Side notes before you read further…
- We are still unsure how our bodies select The Chosen Egg of the cycle but it may have something to do with certain hormonal signaling pathways found specifically in the Dominant Follicle.
- Throughout the menstrual cycle in both ovaries, there are multiple follicles (which are fluid-filled sacs containing your eggs) at different stages of development. Halfway through the menstrual bleed phase (i.e. your period), one follicle in one of the ovaries becomes the largest of all the follicles. The largest follicle is called the Dominant Follicle, and its size is around that of a grain of sand (approximately 1-2 cm or 0.4-0.8 in).
- What happens to the other eggs? A process called atresia happens, wherein the other eggs that grew, developed, but were not ‘chosen’ during ovulation eventually disintegrate.
- Although on rare occasions, a couple of eggs can ovulate at the same time in a cycle. When this happens, there is the potential to conceive fraternal (non-identical) twins if both eggs are fertilized).
Luteal phase – Countdown to the Next Cycle
If the egg is not fertilized, then it disintegrates after 24-48 hours. The Dominant Follicle, after it ruptures, becomes the Corpus Luteum (which literally translates to ‘Yellow Body’ in Latin) after ovulation. The Corpus Luteum is responsible for producing progesterone (and small amounts of estrogen) after ovulation until it also eventually disintegrates. The Luteal Phase of the Ovarian Cycle is named after the Corpus Luteum, and more familiarly it is the phase when progesterone is the ‘dominant hormone’ of the cycle. This phase also generally lasts the same time as the lifespan of the Corpus Luteum, which is around 10-14 days. By the end of the Luteal Phase, progesterone levels dip, which signal your brain and uterus to eventually restart your menstrual cycle via your period.
Quick hormone recap 2:
Your brain produces the Follicle Stimulating Hormone (FSH) and Luteinizing Hormone (LH).
Your eggs (in the ovaries) produce Estrogen in the Follicular Phase, in response to FSH. High estrogen levels and the surge of LH levels trigger ovulation.
After ovulation occurs and the egg disintegrates, the Corpus Luteum (previously the Dominant Follicle) produces Progesterone in the Luteal Phase.
Your uterus: The Uterine Cycle
The changes during the uterine cycle facilitate fertilization, essentially creating an environment where a healthy pregnancy can occur. Like the ovaries, the uterus also goes through its own three phases.
- Menstruation, when bleeding occur (also known as your period)
- Proliferative Phase (Early and Late), and
- Secretory Phase
Menstruation
As you have probably gathered by now, Menstruation is the cyclic sloughing of the endometrial layer of the uterine lining in response to the interactions of hormones produced by the brain and ovaries.
Proliferative phase
The proliferative phase is usually thought of as a singular phase, but it can actually be further studied into two phases – Early Proliferative and Late Proliferative. The Early Proliferative phase is marked by the end of the menstrual flow and a steady rise in estrogen levels. The Late Proliferative phase, on the other hand, is marked by the uterine cells (specifically endometrial cells*) growing in size and number (hence proliferation). The Proliferative phase of the Uterine Cycle occurs alongside the Follicular Phase of the Ovarian Cycle, and both phases prepare for ovulation to take place.
Secretory phase
The Secretory phase happens alongside AND after Ovulation. During this phase, the uterus goes through significant anatomical and physiological changes, much of this is influenced by progesterone, which will ultimately make it possible for an embryo implantation to safely occur within the uterus. With progesterone, the endometrium slows down its proliferation and lining thickness, but increases its vascular supply. The basement membrane of the uterus (called stroma) swells and thickens. While this is happening, the spiral arteries that supply blood flow in the endometrium begin to increase in length and coil, resulting in an increase of endometrial surface area. The endometrial cells also make secretions that are rich in glycogen and glycoproteins.
If fertilization does not occur, then there will be no placental tissue producing Human chorionic gonadotropin (hCG) hormone.* hCG is a hormone involved in supporting pregnancy. Recall from the Luteal Phase that the Corpus Luteum eventually disintegrates and progesterone levels dip. The dip in progesterone levels causes the spiral arteries in the uterine lining to constrict, therefore reducing blood flow to endometrial tissue. This reduction in blood flow causes cell death and the eventual sloughing of the stratum functionalis layer of the endometrium. The shedding of sloughed cells of the endometrium’s stratum functionalis is called menstruation.
Fun facts:
- The endometrium is a layer of the uterus that is thick and has a mucus membrane. There are glands located in the endometrium (also known as uterine glands). These glands produce various substances, such as hormones and growth factors, in the uterus.
- The uterine gland secretions nourish the egg/embryo as it develops in the endometrium.
- hCG helps thicken the uterine lining to support a growing embryo and tells the body to stop menstruation. HCG levels rise after conception and continue to rise until about 10 weeks in pregnancy.
Quick hormone recap 3:
Menstruation occurs and the menstrual cycle begins anew.
To initiate ovulation, your brain produces the Follicle Stimulating Hormone (FSH) and Luteinizing Hormone (LH).
Your eggs (in the ovaries) produce Estrogen in the Follicular Phase, in response to FSH.
Meanwhile in the uterus, with estrogen levels increasing, endometrial cells are proliferating (hence the Proliferative Phase).
High estrogen levels and the surge of LH levels trigger ovulation.
After ovulation occurs and the egg disintegrates, the Corpus Luteum (previously the Dominant Follicle) produces Progesterone in the Luteal Phase.
After ovulation, the endometrium slows down its proliferation stage and becomes more vascularized. Uterine secretions rich in energy-supporting glycogen and glycoproteins are also produced. These changes in the uterus are mainly influenced by progesterone.
The Corpus Luteum eventually disintegrates. If pregnancy does not occur, progesterone nor hCG (made by the placenta) will be present and result in the sloughing of the endometrium’s stratum functionalis layer.
This shedding, accompanied by bleeding, is menstruation, and the menstrual cycle begins again.
Other parts of your body are affected by your menstrual cycle too!
Your body is designed to respond to your hormones AND its fluctuations. You can therefore expect to see changes happening to other parts of your body as you move through different phases of your menstrual cycle.
The Cervix
In the first half of the menstrual cycle (Follicular and Proliferative Phase), the steady increase in estrogen levels also initiates changes in the cervix. Cervical glands produce cervical mucus that tends to be more lubricative (more wet) to better accommodate sperm cells’ survival and facilitate fertilization.
In the latter half of the menstrual cycle (Luteal and Secretory Phase), progesterone decreases and causes the cervical mucus to thicken. The consistency of cervical mucus becomes stickier and non-elastic, and sometimes no mucus is present at all as the latter phase of the menstrual cycle progresses. This change may occur as the fertilization period has passed and sperm entry is no longer a priority.
Body temperature
Estrogen and progesterone have an influence on body temperature, specifically basal body temperature (BBT). BBT is the lowest temperature a person can have during the day and is basically your temperature at rest.
Around the time of ovulation or just before, body temperature is expected to spike slightly (around 0.2ºC or 0.4ºF). This is attributed to the increase of progesterone during this time. Progesterone increases hypothalamic temperature and so the body temperature is significantly increased during the Luteal Phase and Secretory Phases (compared to the Follicular and Proliferative Phases). The increase in body temperature is sustained until the corpus luteum disintegrates and progesterone is no longer produced. If pregnancy occurs, the body temperature stays relatively in the same range, sustained by progesterone production by the corpus luteum (up to ten weeks), placenta, and the ovaries.
Measuring BBT can be a simple, non-invasive, and relatively reliable way of monitoring ovulation, menstrual cycle patterns, and pregnancy (for instance, in recurrent pregnancy losses). You can learn more about BBTs from my other posts [The 1-minute morning routine you can do to take control of your fertility].
What’s normal vs. What’s not normal
For a lot of people, their menstrual cycles are associated with cramping, pain, irritability, depression, bloating, heavy bleeding, unpredictability and a lot of other discomforts. These experiences are common, but are not normal.
What’s normal
The hormonal fluctuations involved (and expected) in your cycle will also influence your experience of your menstrual cycles. That is, your premenstrual symptoms, the length and the heaviness of your menstrual blood flow, the presence of menstrual blood clotting, the length and the predictability of your cycles, the presence of menstrual blood clots, etc. Below is a summary table of what a healthy, ovulatory cycle looks like.
(You can also check out my post on What Healthy Periods are Supposed to be Like for a quicker read that you can bookmark and save for later!)
Period Self-Check
| Premenstrual symptoms | None to mild (manageable) cramping, tiredness, mood changes, appetite changes, skin changes, etc. |
| Menstrual symptoms | None to mild (manageable) cramping, some tiredness (not exhaustion), etc. similar to premenstrual symptoms |
| Cycle length |
25-35 Days During perimenopause, your cycles may be longer or shorter. |
| Menstruation length | 3-7 Days |
| Menstrual blood loss (heaviness) |
The first few days are the heaviest. Changing used/soaked menstrual products (menstrual cup, menstrual pads, tampons, etc.) every 4-6 hours. No more than 6 pads or tampons per day. Around 80 mL of blood loss is considered normal. More than 120 mL of menstrual blood loss may substantially increase the risk of developing anemia from heavy menstrual bleeding. |
| Menstrual tissue clotting | Few strands of tissue |
| Spotting in-between periods | None |
| Ovulation discomfort | None or mild cramping |
What’s not normal and when to worry
If you are concerned that you may have a menstrual disorder or irregularity (see above guide to Period Self-Checks), it is very important to discuss your concerns with your Health Care Practitioner (HCP).
Your HCP will begin with questions about your menstrual concerns. Ideally, details about your other body systems will be asked to get a better understanding of your state of health. In addition to these questions, a physical exam and/or laboratory work-up may be performed and suggested (depending on what their scope of practice is in your jurisdiction). Your HCP may also recommend the following tests:
- Ultrasound – This produces an image of your uterus which can also help determine if there are any abnormalities.
- Sonohysterogram – Fluid is inserted into the uterus through the cervix to examine the uterine lining.
- Endometrial biopsy – This requires a sample of your uterine lining which is taken for testing.
- Hysteroscopy – This involves the insertion of a camera to detect any abnormalities.
When to seek more urgent medical attention
Understanding your menstrual cycle and fully appreciating its complexities can take time. However, there are signs and symptoms that require urgent medical attention as they may indicate a more serious and time-sensitive underlying health problem. Examples of reproductive health emergencies are endometrial cancer, ovarian cancer, uterine cancer, breast cancer, sexually transmitted infections and illnesses, pelvic inflammatory disease, vaginal trauma, ectopic pregnancy, hernia, ovarian cyst rupture, etc.
Look out for the following signs and symptoms and seek urgent care if you are experiencing any of them:
- Abdominal distension or bloating that is persistent
- Early satiety or loss of appetite
- Pelvic or abdominal pain
- Increased urinary urgency or frequency
- Unexplained weight loss or fatigue
- New symptoms of Irritable Bowel Syndrome at >50 years of age
- Presence of abdominal or pelvic mass
- Bleeding after menopause
- Bleeding after sex
- Breast changes such as skin dimpling/puckering, peau d’orange (orange peel) appearance, redness, flaking, nipple inversion (turning inward or pulling in), nipple discharge, new breast lumps (or lump in armpit), change in breast size
- Acute pelvic pain
- Abnormal vaginal discharge (note that discharge is different from cervical mucus)
- Blood in urine
- Low blood pressure
- Dizziness, feeling faint, increased heart rate
Some references for your interest
- Cable JK, Grider MH. Physiology, Progesterone. [Updated 2022 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK558960/
- Critchley, H. O. D., Babayev, E., Bulun, S. E., Clark, S., Garcia-Grau, I., Gregersen, P. K., Kilcoyne, A., Kim, J. J., Lavender, M., Marsh, E. E., Matteson, K. A., Maybin, J. A., Metz, C. N., Moreno, I., Silk, K., Sommer, M., Simon, C., Tariyal, R., Taylor, H. S., Wagner, G. P., … Griffith, L. G. (2020). Menstruation: science and society. American journal of obstetrics and gynecology, 223(5), 624–664. https://doi.org/10.1016/j.ajog.2020.06.004
- Funston, G., O’Flynn, H., Ryan, N. A. J., Hamilton, W., & Crosbie, E. J. (2018). Recognizing Gynecological Cancer in Primary Care: Risk Factors, Red Flags, and Referrals. Advances in therapy, 35(4), 577–589. https://doi.org/10.1007/s12325-018-0683-3
- Holesh JE, Bass AN, Lord M. Physiology, Ovulation. [Updated 2022 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441996/
- Reed BG, Carr BR. The Normal Menstrual Cycle and the Control of Ovulation. [Updated 2018 Aug 5]. In: Feingold KR, Anawalt B, Boyce A, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279054/
- Son, W. Y., Das, M., Shalom-Paz, E., & Holzer, H. (2011). Mechanisms of follicle selection and development. Minerva ginecologica, 63(2), 89–102.
- Thiyagarajan DK, Basit H, Jeanmonod R. Physiology, Menstrual Cycle. [Updated 2022 Oct 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK500020/
If you found this helpful, please feel free to share this article.
Please feel free to send me a message or book an appointment with me by clicking the link on the Navigation Menu above or in the box below if you would like to work together in overcoming your struggles with your menstrual cycles.
Do you need help addressing issues with your menstrual cycles?
Book a Discovery Call with Dr. Kim today to find out how her expertise in integrative medicine can help you!
